Infinity Surgical Associates
For over 15 years our surgeons have been working to provide advanced surgical health care that has helped thousands live longer and happier lives.
Our surgeons, board-certified by the American Board of Surgery, treat a full range of surgical needs from abdominal surgery, gallbladder, advanced breast surgery and hernia repair.
At Infinity Surgical Associates we realize that surgery can often be a daunting prospect, which is why we make every effort to be with you every step of the way. Our friendly and knowledgeable staff work tirelessly to ensure that the warmth and compassion of medical care is not lost in today's world of big-business medicine.
We are committed to doing what's best for your health, and that means taking a conservative approach to your diagnosis and treatment. With advanced training and multi specialty expertise, we can accurately judge which tests or therapies you need and which ones may be unnecessary.
Meet the doctorsWhat We Offer
Emergency Surgical Services Center
24/7 emergency surgical care for acute conditions requiring immediate attention, with experienced surgeons available around the clock.
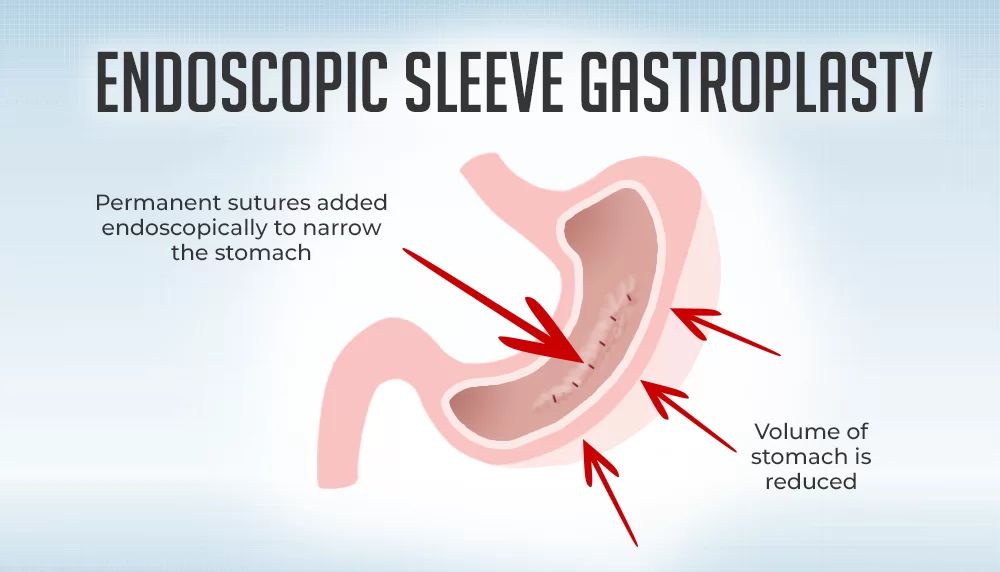
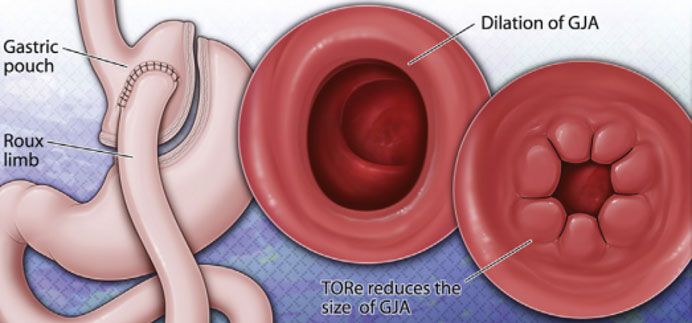
Bariatric Surgery Center
Comprehensive weight loss surgery procedures including gastric band, sleeve gastrectomy, and gastric bypass. Life-changing procedures with proven long-term results.
Thyroid Surgery Center
Expert thyroid surgery using the latest technology including Harmonic Focus ultrasonic shears and nerve monitoring systems to minimize complications.
Hear what our patients are saying!
 My Surgical Testimony for Dr. Alshkaki Osman
My Surgical Testimony for Dr. Alshkaki Osman
Our hope is that when we come out of the surgery we will be better for having gone through it. We begin with identifying the need for the surgery. Finding the right surgeon is generally next on the priority list. Not only is that person going to be responsible for your life, but where he or she practices is key to the decision making process.
The need for surgery in my particular case was growing more evident with each meal. I had packed on the last 70 lbs in three short years. I had tried every possible diet imaginable, and then some. It was just a vicious circle. The more weight I gained, the more depressed I got. The more weight I gained, the more depressed I got. At 270 pounds, it was clear I needed help.
Researching the options available and who offered these options was very involved for me. I had been to other physician's seminars on bariatric surgery, talked to office staff, looked surgeons up online, and met with them. I found Dr. Alshkaki Osman on a bariatric website, We spoke in his office and I was very impressed. He gave me three surgical options and he explained each of them, I took the information home and decided on the gastric sleeve with a non-adjustable band. The option I chose was right for me. I was able, with the help of Dr. Alshkaki Osman, to make the right decision. He explained the surgery fully and wanted to know if I had any questions. He really took the time to make sure I knew what the surgery involved.
George Washington University Hospital is where Dr. Alshkaki Osman performed my bariatric surgery, the professional staff there made me feel like I was top priority. Everyone from the admissions staff to the nurse practitioner was wonderful. Knowing that I was at GW meant that I was in good hands. I believe everyone should have the kind of confidence in their team as I had in mine.

Dr. Alshkaki Osman
Thank you so very much for saving my life.
I am truly grateful for your compassion support and FANTASTIC surgical expertise.
You are a wonderful Doctor and words can't truly express my thanks to you.
From the bottom of my heart, thank you.
Sincerely, Barbara Moore
 Testimonials for Dr. Alshkaki Osman
Testimonials for Dr. Alshkaki Osman
Dr. Alshkaki Osman
Thank you for saving my life and maintaining my life.
You are a good doctor. I feel luck to have met you.
Enjoy these chocolates with your family, for they are the finest too.
Maura K.

Dear Dr. Alshkaki Osman,
I am sooo thankful for everything you have done to help me improve my life drastically!
I've started running in 5k's. Even though I'm not the fastest runner, I'm doing it, and it feels great!
Sarah


 English
English Türkçe
Türkçe العربــية
العربــية